The 45-Second Trick For Dementia Fall Risk
The 45-Second Trick For Dementia Fall Risk
Blog Article
The Main Principles Of Dementia Fall Risk
Table of ContentsSome Of Dementia Fall RiskSome Ideas on Dementia Fall Risk You Should KnowHow Dementia Fall Risk can Save You Time, Stress, and Money.Our Dementia Fall Risk Statements
A loss risk evaluation checks to see just how most likely it is that you will drop. The analysis usually consists of: This consists of a collection of inquiries about your total health and if you've had previous drops or problems with balance, standing, and/or strolling.Interventions are suggestions that might reduce your danger of falling. STEADI includes three steps: you for your risk of falling for your threat elements that can be improved to try to stop drops (for instance, equilibrium problems, impaired vision) to decrease your risk of falling by utilizing efficient methods (for instance, giving education and learning and sources), you may be asked several questions including: Have you fallen in the past year? Are you stressed about dropping?
You'll sit down once more. Your company will check for how long it takes you to do this. If it takes you 12 seconds or more, it might imply you are at greater threat for a loss. This examination checks stamina and balance. You'll being in a chair with your arms crossed over your upper body.
Relocate one foot halfway onward, so the instep is touching the huge toe of your other foot. Move one foot fully in front of the various other, so the toes are touching the heel of your other foot.
Top Guidelines Of Dementia Fall Risk
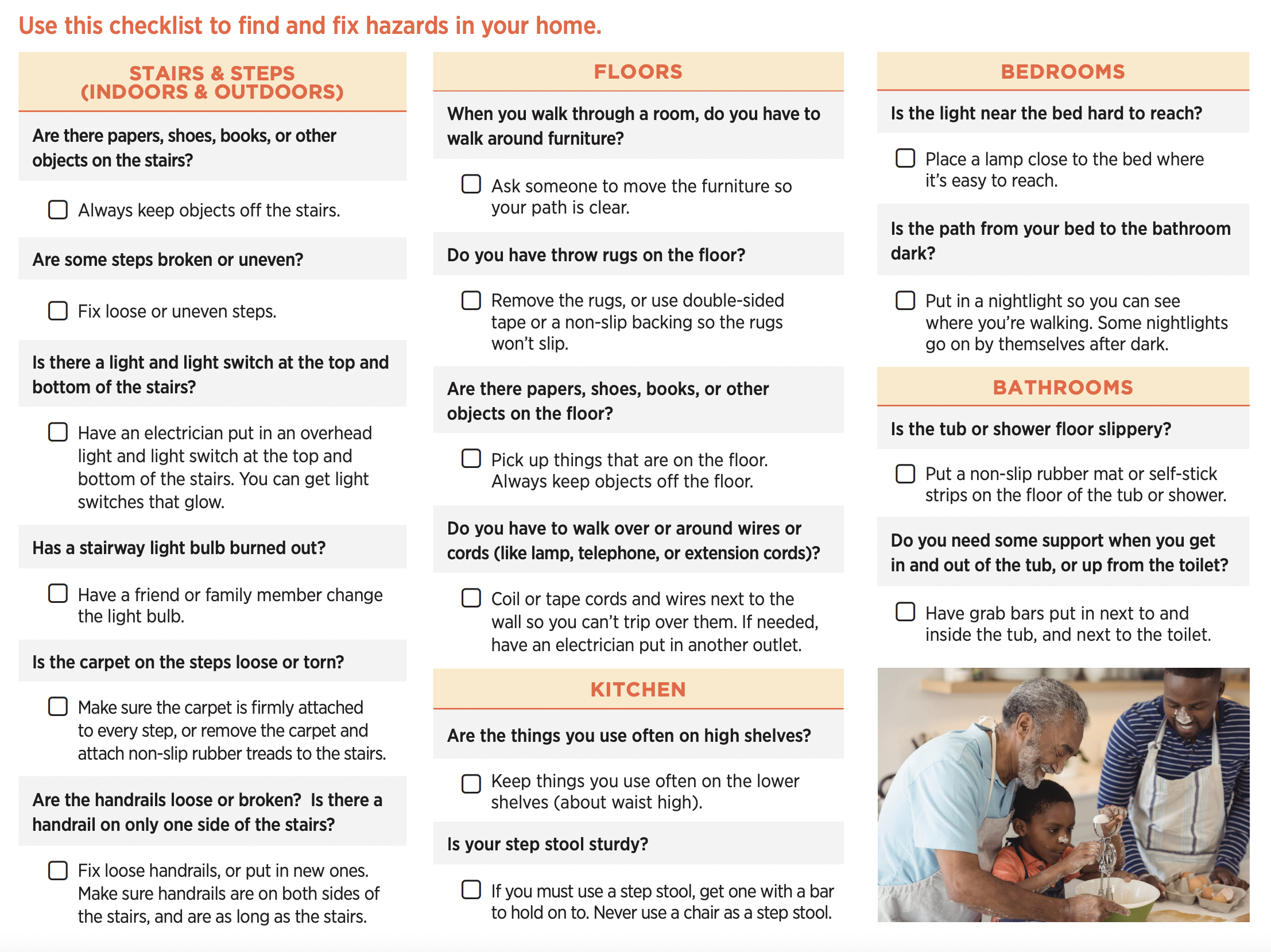
Many drops take place as a result of numerous contributing aspects; therefore, handling the danger of falling begins with recognizing the factors that add to drop risk - Dementia Fall Risk. A few of one of the most relevant risk factors include: History of previous fallsChronic clinical conditionsAcute illnessImpaired stride and balance, reduced extremity weaknessCognitive impairmentChanges in visionCertain risky medications and polypharmacyEnvironmental factors can additionally boost the danger for drops, consisting of: Inadequate lightingUneven or harmed flooringWet or unsafe floorsMissing or damaged handrails and get barsDamaged or poorly equipped tools, such as beds, wheelchairs, or walkersImproper use of assistive devicesInadequate supervision of the people residing in the NF, including those who exhibit aggressive behaviorsA effective autumn risk monitoring program requires a thorough scientific assessment, with input from all participants of the interdisciplinary group

The care strategy need to likewise consist of treatments that are system-based, such as those that advertise a secure environment (appropriate lighting, handrails, grab bars, etc). The effectiveness of the interventions must be reviewed occasionally, and the care strategy modified as needed to show changes in the fall threat analysis. Carrying out a fall threat administration system utilizing evidence-based finest practice can minimize the prevalence of drops in the NF, while limiting the potential for fall-related injuries.
Dementia Fall Risk - The Facts
The AGS/BGS standard recommends evaluating all adults matured 65 years and older for autumn threat yearly. This testing includes asking clients whether they have dropped 2 or his response even more times in the previous year or looked for medical interest for a loss, or, if they have actually not dropped, whether they really feel unstable when strolling.
People who have dropped once without injury must have view their balance and stride examined; those with stride or balance problems ought to get extra analysis. A history of 1 autumn without injury and without stride or equilibrium troubles does not warrant additional evaluation beyond ongoing yearly fall threat screening. Dementia Fall Risk. An autumn threat assessment is required as part of the Welcome to Medicare assessment

Rumored Buzz on Dementia Fall Risk
Documenting a falls history is just one of the top quality indications for fall prevention and management. An essential component of danger assessment is a medication review. Several classes of medications increase fall risk (Table 2). copyright medications particularly are independent predictors of falls. These medicines have a tendency to be sedating, modify the sensorium, and harm equilibrium and gait.
Postural hypotension can commonly be reduced by decreasing the dosage of blood pressurelowering drugs and/or stopping drugs that have orthostatic hypotension as an adverse effects. Usage of above-the-knee assistance pipe and sleeping with the head of the bed boosted may likewise reduce postural decreases in blood pressure. The advisable aspects of a fall-focused physical examination are revealed in Box 1.
A yank time more than or equal to 12 secs suggests high fall danger. The 30-Second Chair Stand test assesses reduced extremity stamina and equilibrium. Being not able to stand up from a chair of knee height without utilizing one's arms indicates raised loss risk. The 4-Stage Balance examination evaluates fixed balance by having the client stand in 4 placements, each progressively much more difficult.
Report this page